In the complex ecosystem of modern healthcare, few devices are as ubiquitous—or as potentially hazardous—as medical needles. These essential tools enable everything from routine vaccinations to complex surgical procedures, yet they simultaneously present significant risks to both patients and healthcare workers. The evolution of safety needle innovations represents one of the most important yet often overlooked advancements in medical technology over the past several decades.
This comprehensive exploration examines how cutting-edge engineering, materials science, and human-centered design are transforming medical sharps safety, dramatically reducing injuries, preventing infections, and ultimately saving lives across healthcare settings worldwide.
The Scope of the Challenge: Understanding Needlestick Risks
Before exploring solutions, it’s essential to understand the magnitude of the problem that safety needles address.
The Statistical Reality
Needlestick injuries present a substantial occupational hazard in healthcare:
- An estimated 600,000-800,000 needlestick injuries occur annually in U.S. healthcare settings alone
- Globally, the World Health Organization estimates that 2 million healthcare workers experience occupational needlestick injuries each year
- Each injury carries potential exposure to more than 20 potential pathogens, including HIV, Hepatitis B, and Hepatitis C
- The direct and indirect costs of needlestick injuries exceed $3,000 per incident in the U.S. healthcare system
- Psychological impact on affected healthcare workers can be substantial, even when no infection occurs
“The statistics tell only part of the story,” explains Dr. Sarah Chen, Director of Occupational Health at Metropolitan Medical Center. “Behind each needlestick incident is a healthcare worker experiencing months of anxiety waiting for test results, potential prophylactic treatments with significant side effects, and in some cases, life-altering infections.”
Risk Factors and High-Risk Settings
Certain clinical environments and procedures carry elevated needlestick risk:
High-Risk Clinical Settings
- Emergency departments with unpredictable patient movements
- Operating rooms with multiple sharps in use simultaneously
- Intensive care units with complex, urgent procedures
- Psychiatric units where patient cooperation may be limited
- Home care settings lacking controlled environments
High-Risk Procedures
- Blood collection and vascular access
- Medication administration via injection
- Suturing and wound closure
- Disposal of used sharps
- Recapping of needles (when still practiced)
The Regulatory Response
Recognition of these risks has driven significant regulatory action:
- The Needlestick Safety and Prevention Act of 2000 mandated safer devices in U.S. healthcare settings
- The European Union’s Directive 2010/32/EU implemented similar requirements across member states
- Comparable regulations have been adopted in Canada, Australia, Japan, and many other nations
- These mandates have accelerated innovation and widespread adoption of safety technologies
- Regulatory frameworks continue to evolve as technology advances


The Evolution of Safety Technology: From Simple Guards to Sophisticated Systems
The journey of needle safety devices spans decades of innovation, with each generation addressing specific challenges in sharps injury prevention.
First-Generation Safety Devices (1980s-1990s)
Early safety innovations focused on simple physical barriers:
- Hinged or sliding needle covers that required manual activation
- Recapping devices allowing hands-free needle coverage
- Needle removal tools for separating needles from syringes
- Puncture-resistant disposal containers
While representing important progress, these early devices had significant limitations:
- Required active user engagement to activate safety features
- Added steps to clinical procedures
- Often awkward to operate, particularly with gloved hands
- Frequently bypassed due to workflow disruption
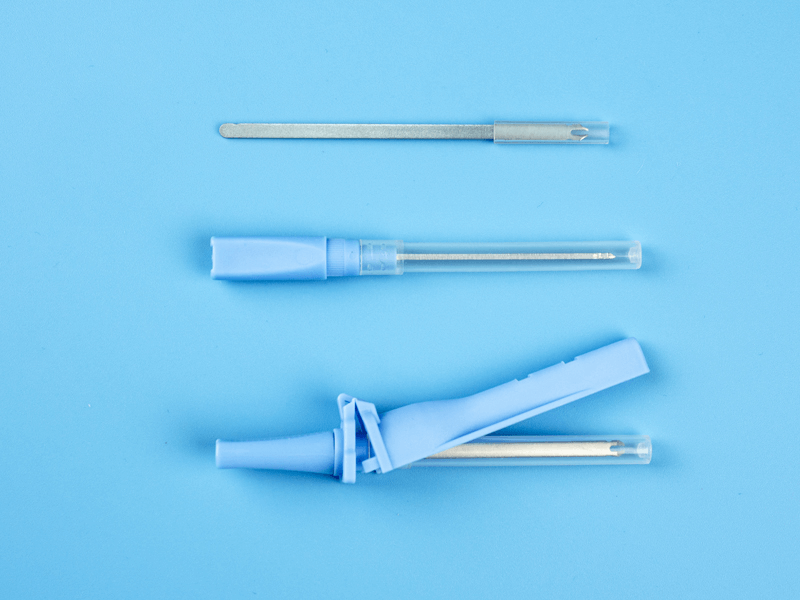
Second-Generation Safety Devices (1990s-2000s)
The next wave of innovation focused on semi-automatic protection:
- Spring-loaded needle shields that deployed with button activation
- Retraction mechanisms triggered by user action
- Self-blunting needles activated after venipuncture
- Needleless connection systems for IV lines
These advancements improved protection but still faced challenges:
- Continued reliance on user activation
- Inconsistent deployment in urgent situations
- Added complexity to device operation
- Higher cost limiting widespread adoption
Current-Generation Safety Technology (2000s-Present)
Modern safety syringes and needles incorporate sophisticated passive protection systems:
Passive Retractable Needle Technology
Retractable needle safety syringes represent one of the most significant advancements:
- Needle automatically retracts into the barrel after injection
- Activation occurs automatically upon complete delivery of medication
- No additional steps required by the healthcare worker
- Needle is fully contained, eliminating exposure risk
- Cannot be reused, preventing potential misuse
“The transition to passive safety technology has been transformative,” notes infection control specialist Maria Rodriguez. “By eliminating the need for user activation, we’ve removed the human factor from the safety equation, dramatically improving protection rates.”
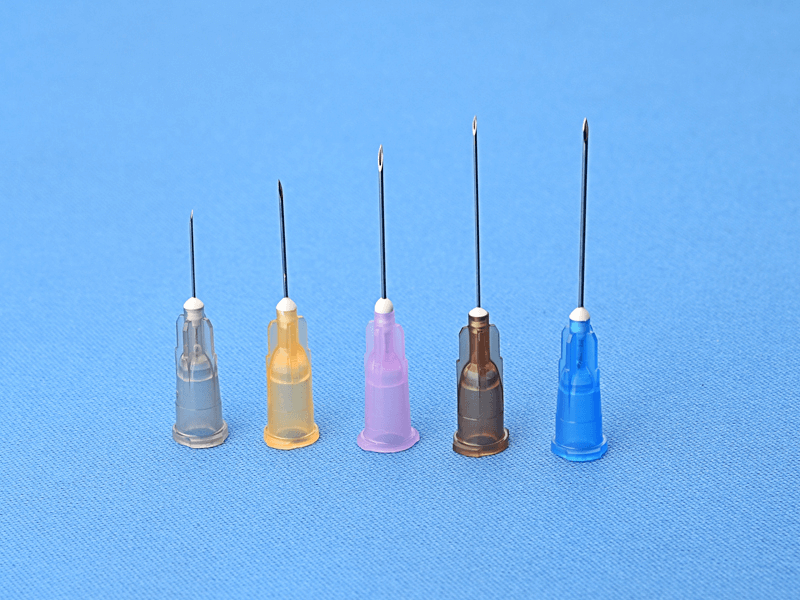
Advanced Shielding Systems
Alternative approaches employ sophisticated protective shields:
- Spring-loaded shields that automatically deploy after injection
- Hinged caps that permanently lock over needles
- Sliding sleeve mechanisms that cover the needle during withdrawal
- Articulating protection arms that encase the needle tip
Specialized Safety Features
Modern devices incorporate additional safety elements:
- Color-changing indicators confirming safety activation
- Audible clicks signaling proper deployment
- Irreversible locking mechanisms preventing reuse
- Transparent shields allowing visualization of medication
Beyond Mechanical Protection: Comprehensive Safety Approaches
While physical protection mechanisms represent the most visible safety innovations, comprehensive needlestick prevention encompasses broader approaches.
Engineered Systems Eliminating Needles Entirely
The ultimate safety solution removes needles completely:
Needleless Connector Systems
IV therapy has been revolutionized by connection systems that eliminate exposed needles:
- Luer-lock connections replacing needle access ports
- Split-septum devices allowing needleless access
- Mechanical valve systems enabling repeated connections
- Positive-pressure connectors preventing blood reflux
Jet Injection Technology
Needle-free injection systems use pressure to deliver medications:
- High-pressure streams penetrating skin without needles
- Consistent delivery depth for reliable absorption
- Elimination of all needlestick risk
- Reduced patient anxiety in needle-phobic individuals
“While not suitable for all applications, needleless technologies represent the gold standard in sharps safety,” explains medical device engineer Dr. James Wilson. “By eliminating the sharp entirely, we remove both the occupational hazard and the disposal challenges associated with traditional needles.”
Material Science Innovations
Advanced materials are enhancing safety through multiple approaches:
Ultra-Thin Needle Technology
Reduced needle diameter improves both safety and patient experience:
- Smaller puncture wounds with reduced bleeding
- Less tissue trauma during insertion
- Decreased pain during procedures
- Faster healing after needle removal
Self-Sealing Port Materials
Specialized materials enhance needleless system performance:
- Silicone formulations allowing repeated punctures
- Antimicrobial-impregnated surfaces reducing infection risk
- Self-healing polymers maintaining integrity after multiple uses
- Clear materials enabling visualization of fluid path
Blunting Technology
Some systems transform needle tips after use:
- Chemical treatments dulling sharp edges
- Mechanical blunting mechanisms activating after injection
- Dissolving needle tips for specialized applications
- Shape-memory alloys changing configuration after use
Specialized Applications Driving Innovation
Several medical specialties have unique requirements driving specialized safety needle development:
Blood Collection Systems
Phlebotomy presents distinct challenges addressed through specialized safety features:
- Retractable needle holders for vacuum tube collection
- Safety adapters for butterfly needle systems
- Integrated holder-needle combinations with automatic safety features
- Blood collection sets with passive needle protection
Insulin Delivery
Diabetes care has spurred numerous innovations:
- Pen needle safety shields automatically covering needles after injection
- Micro-fine needles reducing injection discomfort while maintaining safety
- Integrated safety features compatible with insulin pens
- Needle-hiding designs reducing anxiety while ensuring protection
Surgical Applications
Operating room environments require specialized approaches:
- Safety scalpels with retractable blades
- Protected suture needles with finger guards
- Blunt-tip suture needles for internal closure
- Pass-through zones for safe handling of sharps during procedures
Dental Safety Devices
Dental applications have unique requirements:
- Safety syringes for local anesthetic delivery
- Protected explorers and probes
- Sheathed scalers and curettes
- Needle recapping devices designed for single-handed use

Implementation Challenges and Solutions
Even the most advanced safety needle technology requires effective implementation to deliver its full protective potential.
Overcoming Resistance to Change
Healthcare workers may resist new safety devices due to:
- Familiarity with conventional devices
- Concerns about impact on clinical technique
- Perception of increased procedure time
- Skepticism about safety benefit relative to workflow disruption
Successful implementation strategies address these concerns through:
- Hands-on training with new devices
- Peer champions demonstrating clinical acceptance
- Data sharing demonstrating safety improvements
- Gradual introduction allowing adaptation
Effective Training Approaches
Comprehensive education enhances adoption:
- Simulation-based training mimicking clinical scenarios
- Competency verification before independent use
- Clear visual aids demonstrating proper activation
- Regular refresher training maintaining awareness
Compliance Monitoring and Feedback
Ongoing assessment ensures sustained protection:
- Regular audits of safety device activation rates
- Root cause analysis of any needlestick incidents
- Feedback mechanisms for user concerns
- Continuous improvement processes addressing identified issues
“The technology is only as effective as its implementation,” notes healthcare safety consultant Robert Chen. “Even the most sophisticated safety device will fail to protect if it’s not used correctly or consistently. Successful facilities recognize that implementation is an ongoing process, not a one-time event.”
Economic Considerations: The Business Case for Safety
While the human cost of needlestick injuries provides compelling justification for safety technology, economic analysis further strengthens the case for implementation.
Direct Cost Analysis
Comprehensive economic assessment includes multiple factors:
Needlestick Injury Costs
- Immediate testing of source patient and injured worker
- Post-exposure prophylaxis when indicated
- Follow-up testing over monitoring period
- Lost work time during evaluation and treatment
- Workers’ compensation claims
- Potential litigation expenses
Safety Device Investment
- Acquisition premium over conventional devices
- Training and implementation costs
- Disposal system modifications if required
- Ongoing compliance monitoring
Return on Investment Calculations
Multiple studies demonstrate favorable economics:
- A comprehensive analysis published in the Journal of Healthcare Risk Management found that safety device implementation yielded a 3.5:1 return on investment over a three-year period
- Facilities typically recoup initial investment within 12-18 months through reduced injury-related expenses
- Larger healthcare systems report annual savings of $250,000-$400,000 after full implementation
- Reduced insurance premiums often follow improved safety records
“The economic case for safety devices has been conclusively demonstrated,” explains healthcare economist Dr. Michael Brown. “What was once viewed as a cost burden is now recognized as a sound financial investment with returns extending beyond direct cost savings to include staff satisfaction and retention benefits.”
Global Perspectives: Safety Across Healthcare Systems
The implementation of needle safety devices varies significantly across global healthcare systems, influenced by regulatory frameworks, economic resources, and cultural factors.
High-Income Countries
Advanced economies typically feature:
- Comprehensive regulatory mandates for safety devices
- Near-universal implementation in acute care settings
- Growing adoption in ambulatory and long-term care
- Ongoing innovation driven by competitive markets
- Sophisticated surveillance systems tracking outcomes
Middle-Income Nations
Emerging healthcare systems demonstrate:
- Increasing regulatory attention to sharps safety
- Targeted implementation in high-risk settings
- Growing domestic manufacturing reducing cost barriers
- Public health campaigns raising awareness
- Phased approaches prioritizing highest-risk procedures
Resource-Limited Settings
Challenging environments require creative approaches:
- Focus on highest-risk procedures when resources limit universal implementation
- Emphasis on training and administrative controls
- Innovative low-cost safety device development
- International partnerships supporting technology transfer
- Integration with broader infection control initiatives
“The global disparity in access to safety technology represents one of the most significant equity issues in healthcare worker protection,” notes Dr. Elena Vasquez, international health consultant. “Bridging this gap requires not just technology transfer but contextually appropriate implementation strategies that recognize the realities of diverse healthcare settings.”
Future Directions: The Next Generation of Protection
The evolution of safety needles continues, with several emerging technologies poised to further transform sharps safety.
Smart Connected Devices
Digital integration is accelerating:
- NFC and RFID-enabled devices tracking usage and disposal
- Bluetooth connectivity to healthcare systems
- Integration with electronic health records
- Real-time monitoring of compliance rates
Novel Material Applications
Advanced materials are enhancing performance:
- Silicon microneedle arrays for painless delivery
- Shape-memory alloys enabling novel safety mechanisms
- Antimicrobial materials reducing infection risk
- Biocompatible polymers reducing inflammatory response
Alternative Delivery Routes
Beyond traditional injection:
- Microneedle patch technologies
- Dissolving needle platforms
- Inhalable and transdermal alternatives for traditional injectables
- Oral delivery systems for traditionally injected medications
Artificial Intelligence Applications
AI is enhancing safety through:
- Predictive analytics identifying high-risk situations
- Computer vision systems detecting unsafe practices
- Machine learning optimizing device design
- Natural language processing improving incident reporting
“The next frontier in sharps safety will likely involve the integration of digital technology with physical protection,” predicts medical technology futurist Dr. James Chen. “By creating smart, connected devices that not only protect but also monitor and report, we’ll move from passive safety to proactive risk management.”
Case Study: University Health System Implementation
The experience of University Health System, a multi-hospital network with over 15,000 employees, provides valuable insights into comprehensive safety implementation.
Initial Assessment
The organization conducted a thorough baseline evaluation:
- Analysis of three years of needlestick injury data identifying high-risk areas
- Comprehensive device inventory across all clinical settings
- Staff surveys assessing perceptions and concerns
- Economic impact analysis of existing injury patterns
- Regulatory compliance assessment
Strategic Implementation
The system adopted a phased approach:
- Formation of multidisciplinary selection committee including frontline staff
- Standardized evaluation criteria for all potential safety devices
- Clinical trials of finalist devices in representative departments
- Comprehensive training program developed before full deployment
- Phased rollout beginning with highest-risk areas
Ongoing Monitoring
Sustained attention ensured continued success:
- Monthly tracking of needlestick injury rates by department
- Regular compliance audits of safety feature activation
- Feedback mechanisms for staff concerns
- Annual reassessment of available technology
- Continuous improvement process addressing identified gaps
Measured Outcomes
After 24 months, the system reported:
- 78% reduction in needlestick injuries system-wide
- 94% decrease in high-risk exposures involving known infected patients
- Estimated $380,000 annual savings in direct and indirect costs
- Significant improvement in staff satisfaction scores
- Recognition as a safety leader by regulatory agencies
“Our experience demonstrates that successful implementation requires more than simply purchasing safety devices,” notes Robert Park, Chief Safety Officer. “It demands a comprehensive approach including careful selection, thorough training, ongoing monitoring, and continuous improvement. The dramatic results justify the investment in both financial and human terms.”
Conclusion: The Future of Medical Sharps Safety
The evolution of safety needle innovations from simple guards to sophisticated passive protection systems represents one of the most significant yet often overlooked advancements in healthcare worker protection. As these technologies continue to develop, they promise to further reduce the incidence of needlestick injuries, prevent bloodborne pathogen transmissions, and ultimately save lives among those who dedicate themselves to patient care.
For healthcare facilities evaluating safety technology, the evidence is clear: comprehensive implementation of modern safety devices delivers measurable benefits in human, clinical, and economic terms. The question is no longer whether to implement safety technology, but rather how to select and deploy the most appropriate solutions for specific clinical environments.
In the words of Dr. Chen: “When we discuss healthcare safety, we often focus on patient protection—and rightfully so. But the protection of healthcare workers through technologies like safety needles represents an equally important ethical imperative. By investing in these devices, we’re not just preventing injuries; we’re demonstrating our commitment to those who provide care at the frontlines of medicine.”
This article is part of our comprehensive series on essential medical equipment. For more information on related topics, including surgical lights, exam lights, cold light sources, and integrated medical device solutions, explore our complete resource library.

